The release of the preliminary report of the second Kenya AIDS Indicator Survey (KAIS 2012) received wide coverage in the print media in Kenya.
They agreed that most of the stories in the media failed to understand what the numbers mean. But the most misleading was a story published in The Standard with the title: Push for male circumcision in Nyanza fails to reduce infections.The main misrepresentations of data in the story were:
- The unfounded assumption that male circumcision would have a population-wide impact so quickly. Kenya launched a national program of voluntary medical male circumcision (VMMC), in November 2008. It is not expected to make a significant difference in prevalence (where many factors are involved) until about 2025.
- The writer of the story forgot that Nyanza had a much higher prevalence to start off with (much more than other regions) – so no single intervention is going to bring the prevalence to the same level as other regions, for many reasons. It also did not consider that with more HIV positive people accessing antiretroviral drugs many of them are living longer and this could lead to a higher prevalence of HIV compared to just a few years ago when the lifespan of an infected person was much shorter so the total number of surviving infected people at any one time would have been lower.
Some of the story ideas journalists can explore based on the report include:
Increased testing: The proportion of HIV positive people who were aware of their HIV status tripled from 16 per cent in 2007 to 47 per cent in 2012.
Shift in age group: The age group 45 – 54 years had the highest HIV prevalence at 9.1 per cent, compared to age group 25 – 34 years in 2007. Is this generation that had the highest HIV prevalence seven years ago still the highest now – only that they have aged into an older age group? Is this an indicator that HIV will eventually be phased out if the trend continues?
Link between formal education and HIV: Men and women who completed secondary education had a higher rate of HIV infection than those who had not attended primary education. Why? Have HIV prevention campaigns left out the educated? Is stigma higher among the educated than the less educated?
The following is the response of the National AIDS and STD Control Programme VMMC programme manager, Dr Athanasius Ochieng’ to The Standard story.
"The preliminary report of the second Kenya AIDS Indicator Survey (KAIS 2012) released on September 10 this week shows that significant progress has been made in HIV prevention, care and treatment in Kenya.
Nationally, HIV prevalence — which represents the percentage of adults aged 15 to 64 years infected with HIV — dropped from 7.2 percent in 2007 to 5.6 percent in 2012.
Among the HIV prevention efforts that the Government of Kenya and its partners have implemented in the past five years is voluntary medical male circumcision (VMMC). Conclusive studies have shown that getting circumcised reduces a man’s chances of becoming infected with HIV through vaginal sex by about 60 percent.
The survey found that the more than 600,000 boys and men circumcised nationally represent a six percent increase in male circumcision prevalence over five years, from 84 percent to 91 percent. The Nyanza region recorded the highest increase, from 48 percent to 66 percent.
This progress is encouraging, but it shows that greater effort is needed to provide services to all men who wish to be circumcised. The national VMMC strategy is based on mathematical modeling studies showing that in the Nyanza region alone, circumcising 80 percent of sexually active uncircumcised men aged 15 to 49 years by the end of 2013 would prevent an estimated 900,000 infections among men and women by 2025.
Impact of male circumcision
In Nyanza, HIV prevalence held steady at 15 percent from 2007 to 2012. The Standard’s story on the KAIS 2012 mistakenly assumed that this finding reflects the effects of recent efforts to scale up VMMC services. But it is too soon to see the impact of male circumcision on HIV prevalence, for a number of reasons.
Mathematical models show that the impact of higher rates of male circumcision on
HIV prevalence increases over time, particularly among women. As reduced risk among circumcised men leads to fewer HIV infections, the risk of exposure to the virus declines for the entire population.
HIV prevalence is affected by both new infections – which add to prevalence — and deaths of HIV–infected individuals – which subtract from prevalence. We do not expect HIV prevalence to drop as fast as new HIV infections, because our HIV and AIDS treatment program is helping so many people with HIV live longer, healthier lives.
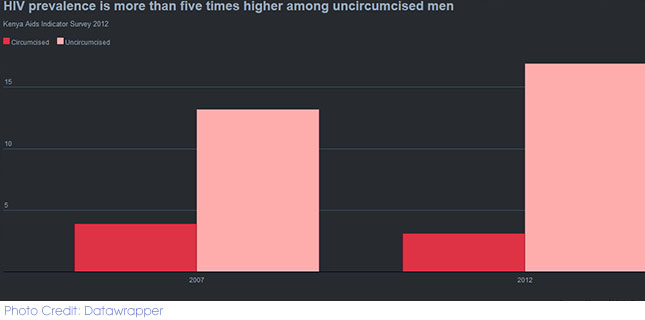
It is worth noting the KAIS 2012 finding that HIV prevalence is more than five times higher among uncircumcised men: 17 per cent of uncircumcised men are infected with HIV, compared to three percent of circumcised men. A recent study conducted in a South African community that is scaling up VMMC for HIV prevention found that VMMC was responsible for reducing new HIV infections by at least 57 percent.
Comprehensive HIV prevention
Male circumcision gives men partial — but not complete — protection against HIV infection. That is why VMMC is provided along with counseling about how to reduce one’s risk of HIV, condoms and instructions on their use, screening and treatment for STIs, and the offer of HIV counseling and testing.
Concerns that men might take more risks after circumcision have not been borne out so far. Studies in Nyanza have found no increase in risky sexual behavior after male circumcision and no differences in behavior between circumcised and uncircumcised men. Studies in other countries have reported similar findings. The VMMC programme continues to study the question and to encourage clients to continue practicing safe sex.
Redoubling our efforts to reach as many men with VMMC services is critical as we work towards getting to zero infections."
To further explore how to analyze and find stories in data contact us at: datadredger@internews.org